I have gastroparesis.
Gastroparesis is a condition that affects the normal spontaneous movement of the muscles (motility) in your stomach. Ordinarily, strong muscular contractions propel food through your digestive tract. But if you have gastroparesis, your stomach’s motility is slowed down or doesn’t work at all, preventing your stomach from emptying properly.
For me, how it feels varies from day-to-day or even minute-to-minute. Sometimes it feels like what I eat gets stuck in the middle of my chest. I’ll develop nausea out of nowhere, nausea that ranges from annoying to debilitating. I’ve had projectile vomiting. Or I’ll experience a severe burning sensation that feels like my insides are eating themselves. Sometimes I’m able to taste what I had for breakfast while trying to fall asleep. I’ve also had the pleasure of having my breakfast come back up my throat when I lay down to go to bed. Yuck.
BUT… I’m thankful to say that I now have many days when my symptoms are just a minor annoyance instead of debilitating. For the average person, the stomach should be empty within 3-4 hours. My nuclear stomach emptying study showed I had 76% left in my stomach 4 hours after eating scrambled eggs and toast. One doctor documented that this is a “very convincing gastric emptying study” and another said I have “one of the worst gastric emptying studies I’ve ever seen.” My favorite response from a provider is “I thought the gastric emptying time in your records was a typo.” Even so, I get the impression that my symptoms are not as severe as others. So what works for me, might not work for others.
I would like to give a shout out to my gastroenterologist for referring me to Virginia Mason’s gastroenterology group. Not only do they have one of the world experts on gastroparesis, they also have a nutritionist on staff that provides free consultations. The free part is awesome, but what’s even more awesome is that she cares for a lot of gastroparesis patients and can offer suggestions based on what has worked for others.
In this post, I’m going to talk about the medication, diet/eating approach that is working for me. I plan to follow-up with a post about lifestyle changes and how changing how you eat impacts social interactions.
UPDATE: the week after initially publishing this post my gastroparesis flared up, so I’ve updated with some additional tips.
MEDICATIONS
Schedules/Daily Meds
These are the medications I use to prevent symptoms.
- PPI to control acid. I take lansoprazole simply because that is what I bought over-the-counter when I first became symptomatic and no provider has recommended switching because this currently works for me
- Ranitidine. I added this to my daily meds (I only need it in the AM) in the fall when the lansoprazole wasn’t cutting it on its own. I can’t tolerate the pain without both meds, which is disappointing because both can cause hair loss.
- Miralax. My “gastric dysmotility” extends beyond my stomach to the rest of my gut. So constipation is a factor. I didn’t find much relief with magnesium supplementation (although I still use it). Instead, I use 1/8-1/2 tsp of Miralax in my morning protein shake (I was told to dilute in 12-18 oz of water for best effectiveness).
- Multivitamin. To prevent nutritional deficiencies associated with gastroparesis.
- When my gastroparesis flares, I don’t tolerate tablets, so right now I’m using Centrum chewables.
- I also tolerate the Isagenix women’s multivitamin
PRN / As needed Meds
These are what I use to control symptoms. Sometimes I can’t tell if I am nauseated, having heartburn, or am hungry. So I just go through the options until I get relief.
- my #1 lifesaver: TummyDrops!
- I love these and try not to leave the house without them. I hate eating out and then feeling miserable and having nothing with me.

- I use the Ginger Pear drops for mild nausea and the Double Ginger Peach for more severe nausea or if it feels like what I ate is “stuck.” If I’m having a “bad” day, I sometimes use one before I eat to get my stomach moving. I like that they are hard candy so I can pop it in my mouth and go without having chewy ginger candy stuck to my teeth.
- Ginger water was also recommended, but I haven’t tried it
- I tried making my own ginger candy, but it was time-consuming and it went bad before I used all of it.
- Tip for making your own ginger-related remedies is to drop the ginger in boiling water for 10 seconds to make the skin easier to remove
- I love these and try not to leave the house without them. I hate eating out and then feeling miserable and having nothing with me.
- #2 eat something that I normally tolerate
- #3 Mylanta
- If you want to use Mylanta, don’t do the generic brand plain flavor 🤮. The minty one is decent. I’m about to try the Vanilla Carmel and hope it doesn’t ruin those flavors for me forever.
- Others have success with different antacids, but I respond better to magnesium and aluminum.
- #4 Reglan. I try to avoid this until I absolutely have to take it. And I only do 1/2 tab. This is basically my “I’ve done everything and I still feel so terrible I can’t go to sleep” solution. I’m prescribed enough to use daily, but I typically use it once a week or less. But I always try to keep some on me because sometimes the need to vomit hits me out of nowhere and it responds to nothing except Reglan. And working or doing normal daily activities are really challenging when you feel like you have a stomach bug or the flu.
- Why do I avoid it if it works so well? Reglan has some side effects that I want to avoid and I’ve been told if I develop them (EPS or extrapyramidal side effects) I have to stop using it. My understanding is that the likelihood of a reaction is related to how much/frequently I use it.
- Note: one of the things that helped point us to a gastroparesis diagnosis was because Zofran doesn’t work AT ALL, but Reglan does. Zofran still works for nausea with other causes (i.e. gastroenteritis or influenza)
Pain meds
I’m no longer able to tolerate ibuprofen, which was my go-to options for pain management. So now I use acetaminophen and a supplement called Curamin as needed.
THINGS TO AVOID
Overeating
Nausea is a powerful deterrent / negative reinforcement. So, I quickly learned that overeating was a recipe for feeling horrible. When I feel full I have to stop right then. Even “one more bite” is enough to ruin the rest of my day.
Irritating Foods
I’m pretty disciplined about avoiding foods that irritate and/or slow gastric emptying. With food lingering in my stomach for hours I develop gastritis pretty easily (which is inflammation of the stomach lining… it’s a painful, burning sensation that feels like my stomach is eating itself).
Here are the foods I avoid:
- Coffee. even decaf. This makes me sad because I love the taste.
- Acidic foods including tomato sauces. I miss spaghetti and lasagna!
- Citrus. I still put citrus juice in recipes, but I am careful with the amount.
- Fried and/or high-fat foods. Fat slows down gastric emptying. But I still have the occasional order of french fries
- Soy. I found that soy makes my symptoms worse. I can tolerate small amounts but mostly avoid all but soy lecithin.
- Chocolate 😭… but only when I have flares
I tried removing dairy, but that didn’t seem to make a difference and including dairy provides a lot of additional, easy to eat options. I was gluten-free prior to this diagnosis.
RESOURCES
Here are PDFs of handouts that I received that are very helpful. I recommend reading them. I discovered a lot of the info in these handouts by trial and error. I wish I had access to them earlier (instead of 2 years after my initial diagnosis)
- Diet interventions for gastroparesis by University of Virginia Health System Digestive Health Center of Excellence
- Gastroparesis diet guidelines by Virginia Mason
- Balanced snacks by Virginia Mason
Other resources I discovered while writing this blog
- Gastroparesis Patient Association for Cures & Treatment Inc (G-PACT)
- The Gastroparesis and Dysmotility Association (DPDA)
- American Neurogastroenterology & Motility Society
- National Organization for Rare Disorders
SHAKES
I have experimented with multiple eating plans:
- five shakes a day plus one meal
- two shakes a day (beginning and end of day) plus two snacks and one meal
- one shake a day, 1-2 meals and 2+ snacks depending on how hungry I am / activity level.
I vary my eating based on how I feel and what I’m doing that day. But one thing I don’t mess with is how I start my day.
On the rare occasion where I decide to start with something other than a shake, I end up regretting it. I call these “dietary indiscretions”
***Morning Shake***
 I start every day with a protein shake that includes collagen and Miralax. I like to mix my shake with a milk frother, I get fewer clumps than when using a protein shake bottle and I can drink my shake in a mug (fewer pieces to wash! yay!). This provides enough sustenance for my stomach to tolerate my morning meds and supplements.
I start every day with a protein shake that includes collagen and Miralax. I like to mix my shake with a milk frother, I get fewer clumps than when using a protein shake bottle and I can drink my shake in a mug (fewer pieces to wash! yay!). This provides enough sustenance for my stomach to tolerate my morning meds and supplements.
- I supplement with vitamin D, multivitamin, biotin and collagen (also for the hair loss), magnesium, and omega/fish oil. This is based on blood lab results and recommendations from my doctors based on my health.
- Burping fish oil is nasty. If you need fish oil, I like these burpless fish oil capsules.
The texture and taste of whey protein shakes are WAY better than pea protein. However, not all whey protein is created equal. My all-time favorite is Isagenix Peach Mango. I could drink that every day multiple times a day. Unfortunately, it’s pricey. Orgain branded protein shakes were recommended by my nutritionist and I like them (some varieties are even carried at Costco). When I’m tolerating chocolate, the shake I use the most is Chocolate Orgain Whey Protein Powder.
Here are some flavor combinations to break up the monotony:
- Orgain Natural Unsweetened protein powder OR plain whey protein PLUS either water or almond milk PLUS
- 1 Tablespoon Jello sugar-free pudding powder (I like banana, butterscotch, pistachio, vanilla, white chocolate. Lemon was disgusting)
- Sometimes I like to combine the White Chocolate SF pudding powder with 1 scoop of JUCE (super fruit and veggie powder)
- Or I’ll combine the pistachio pudding powder with a scoop of powdered green stuff
- Orgain chocolate protein powder + Powdered Peanut Butter
- Sometimes I add banana pudding powder to this combo (yum!!!)
- For chocolate protein powder I have 3 varieties I use:
- protein powder mixed with almond milk
- chocolate meal mixed with water
- 1 tsp cocoa + unsweetened plain powder
- I don’t like the Orgain vanilla protein powder taste, so when I had a container I wanted to finish, II added 1/2 packet of Splenda + 1/2 tsp cinnamon and/or 1 tsp cocoa and/or 1 tsp vanilla abstract
I was inspired to mix flavorings by proteinpow.com
DAILY MEAL
Meal Timing
I eat my main meal around lunchtime. This is when my stomach seems to work the best. I feel like my stomach takes several hours to “wake up” in the morning. And then I need to finish eating 3-4 hours before going to bed (since we want gravity to help with stomach emptying), so that makes dinner challenging especially when I’m working 12-hour shifts.
Typically, I only eat 1 main meal per day, the rest of my nutrition comes from smaller (100-200 calorie) snacks spaced throughout the day
Meal proportions
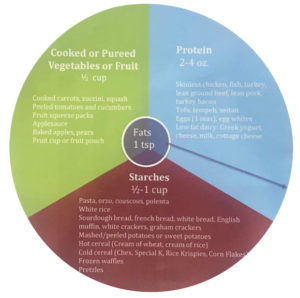
Gastroparesis Plate
The recommended “plate” for gastroparesis, is 1/3 protein, 1/3 starch, 1/3 cooked/pureed veggies and/or fruit.
I try to do 1/4 lean protein + 1/4 complex carbohydrates + 1/2 fruits and veggies, which is what I learned to do when losing weight with Isagenix (which is very effective for healthy weight loss, especially abdominal fat, but also very expensive).
But to be honest, my meals are often higher on the starch/carbs and lower on the fruits/veggies. I may start adding JUCE (super fruit and veggie powder) to my daily shake to increase my micronutrient intake.
I love using sweet potatoes as my complex carbohydrate. It’s easy to digest, tastes delicious and is great left over.
 It never occurred to me to look for gastroparesis recipes or cookbooks, but my nutritionist recommended The Gastroparesis Cookbook by Karen Frazier. (update: After seeing this post my Mom bought me this cookbook. I LOVE it. It clearly indicates which recipes are GERD-friendly, SIBO-friendly, gluten-free, etc. Plus it has great information and tips for managing gastroparesis. I HIGHLY recommend it!)
It never occurred to me to look for gastroparesis recipes or cookbooks, but my nutritionist recommended The Gastroparesis Cookbook by Karen Frazier. (update: After seeing this post my Mom bought me this cookbook. I LOVE it. It clearly indicates which recipes are GERD-friendly, SIBO-friendly, gluten-free, etc. Plus it has great information and tips for managing gastroparesis. I HIGHLY recommend it!)
SNACKS
I work 12 hour days, so I pack a lot of snacks. Here are my main go-to options.
- string cheese and/or low-fat baby bell cheese (fat decreases gastric emptying, so low-fat options work best. I think low-fat string cheese has a weird texture)
- Chobani fat-free Greek yogurt + honey (sometimes I use real maple syrup instead and/or add berries and/or granola)
- Citterio Genoa + Provolone (Costco or Trader Joe’s)
- 1/2 protein bar (protein bars may be too dense for your stomach, so be careful)
- I occasionally use Isagenix bars. I like the chocolate peanut crunch (favorite because it keeps me satiated), chocolate decadence, chocolate crisp.
- Rx bars was another recommendation but I haven’t tried them since developing gastroparesis.
- Homemade almond butter on GF bread. I put 1.5 cups of raw almonds and 1 tablespoon of extra virgin olive oil or almond oil into my Blendec twister jar. It takes less than 1 minute.
When my stomach cooperates, I like to include raw nuts and raw fruits/veggies. When my gastroparesis flairs, I don’t eat these.
 peanut butter and apple
peanut butter and apple- hummus + celery (I avoid spicy hummus because spicy foods increase gastritis and acid reflux.)
- Epic bison bars (I get them at Trader Joe’s)
- a small handful of almonds (only if your stomach tolerates them. I buy the mini packs at Trader Joe’s when I can)
- For more ideas check out Balanced snacks by VM, however, not everything on this list is gastroparesis-friendly
FUTURE OPTIONS
Thankfully my team has provided me with options should my symptoms increase/become unmanageable.
Supplements & Medications
- FDguard. I’m ordering some now and will see how it goes. (update: Unfortunately, I noticed no difference when using this)
- Domperidone. I plan to get some next time I’m in Canada (update: turns out my MD is no longer allowed to prescribe medications not approved for use by the FDA)
- Erythromycin. We haven’t tried this as my symptoms are controlled and its efficacy can wane with long term use. We want to keep this option available if my symptoms become worse / result in a hospitalization
- Wheat Dextrin. It’s gluten-free despite the name. This is on my list of options if Miralax doesn’t “do the trick.” What’s cool about it (unlike Miralax which can only take you from constipated –> soft –> WAY TOO SOFT) is it can be used for both constipation and diarrhea. For constipation, it is added to water and for diarrhea, it can be sprinkled on food.
Surgical options
If we get to the point where my symptoms are unmanageable, I’ve been told I have these options:
- Gastric POEM
- Pyloric Botox injections
- PEG-J (Gastro-jejunostomy tube)
- Enterra Neurostimulator (Personally, I’ve placed this in my “absolutely last-ditch solution” bucket)
Unfortunately, not every gastroparesis patient is the right fit for these options.
In my research, I discovered some other options for gastroparesis associated with GERD: nissen fundoplication and Stretta.
TOP TIPS
If you take nothing else away from this blog:
- Try TummyDrops. Serious, these candies keep me living the life I want to live.
- Avoid overeating
- Figure out what foods work for you
- Stay AWAY from what foods that irritate your stomach. Just don’t do it. I know it’s tempting… but that bite is not worth it.
- Start your day with liquid foods
- Eat your main meal in the middle of the day
- Work with your care team to find a medication combination that works for you
CLOSING & DISCLAIMERS
I hope this was helpful. And I’d love to hear tips that others with gastroparesis have discovered. Please comment or message me!
This post is not meant to replace medical consultation and advise. I am simply sharing my experiences with managing the day-to-day pain and discomfort of gastroparesis in the hope of encouraging others and providing access to the information/resources I wish I had encountered sooner.
This post contains NO affiliate links. I’m only including links to products because I want to make it easy for others to find options that work for them. If you’re interested in using any of the Isagenix products, I know a great coach (who is not me!).


Thank you so much for this very informative post. I’ve struggled with gastroparesis for over 10 years, and I am excited to try adding some of your tips to my routine.
I’m glad to hear you came away with some ideas! I’d love to hear how it goes!
My daughter suffers from this and she has horrible stomach pain is there anything you can suggest for the pain
I’m sorry I didn’t see your comment until now, Tami. I’m sorry she is having pain. There are different types of pain with gastroparesis. Mine was related to acid reflux so taking a Proton Pump Inhibitor and finding the right over the counter antacids worked for me. I also had pain from my stomach being distended, and the ginger candies and Reglan helped my stomach empty. But ultimately it’s important to find a GI doctor that can help find the right treatment combo for her. Wish you the best
I went plant based vegan and cut out dairy, refined sugars and meat. This helped me tremendously! No more pain, herbs i take being plantbased has assisted with digestion, no more GERD or gastroparesis in a year.
What herbs?
I have these products I question. Complete by Juice plus. Whole Foods based shake mix. French vanilla. Whole food based shake mix Further FOod Collagen Peptides I don’t know much about this diet. I will try to find the TummyDrops
Where do I find the TummyDrops.
I’m sorry I’m just now seeing your comment. I buy them on amazon
I loved your information here. I was diagnosed with gastroparesis about a year ago and have been struggling from day to day trying to figure out what will and wont work for me.
I must say its a process… My main struggle has even dealing with the (what seems) like constant bloating. Very uncomfortable!
I take Creon (meds from my gastro dr)with everything I eat. It has been great with very few flareups.
I am eager to see how I do with hummus… I didn’t realize I could still have it. I know chickpeas ate difficultt to digest so I just wrote off hummus… But I’m going to give it a go!
Thank you for all the great info, and best wishes to you on your journey with gastroparesis.
How did the hummus go?
Hi Krista, I just want to let you know that you have helped me tremendously because I had an appt with a surgeon Tuesday about a gastric pacemaker and it scared me to death with all the cutting and I said no, I have another appt Friday about the Per Oral Endoscopic Pyloromyotomy and I have already made a decision to not do anything except what you are doing, I want to learn to live with this because I don’t think I’m as bad as a lot of people I see in my group on Facebook, but after reading your article you have inspired me to take care of myself in the best way possible without surgeries or endoscopic procedures so I just want to thank you and you give me courage to walk this journey!…..Lori
Hi Lori, I’m sorry you’re dealing with gastroparesis! I hope that you find the right routines for your body. I’ve had to adjust mine over time and not everyone tolerates the same things I do. I think what helps me the most is figuring out which medications help which symptoms and taking them as soon as I have symptoms. I wish you all the best!
Hi Krista, I am having a gastric emptying test this week. My symptoms mimic yours completely, but I’m wondering if you had a regurgitation problem also! I have a history of digestive issues including IBS and gastritis. I drink a non dairy protein drink in the morning and nibble on banana and jello for lunch. I seem to tolerate eggs ok but if I add anything to this I get what feels like food in my upper chest and I just bend over and it comes out, mostly digested but like cloudy looking with some liquid-y food. Your site gave me hope – I’m so panicked what my eating future holds! I haven’t been diagnosed as yet but my symptoms are GP-ish. Thank you for posting this very informative blog! Wish you had Instagram!
Hi Lynn. I’m sorry you’re having these symptoms but glad you’re on the route towards a diagnosis. When I was diagnosed, I was having regurgitation… food would come into the back of my throat when I laid down. I’m on Instagram but don’t use it very often: @kristajoyv
Thank you so much for your fast reply! I’m hoping that’s not what I have (I do poop a lot after eating especially if I put 1/2 tsp flax in my protein shake). Hoping that’s a good sign 😀
Hello! First of all, I’m so glad that I found your blog post, gives me so much hope on handling my GP better.
I have post-bowel surgery gastroparesis, been diagnosed for almost 2 years. The main issue that I am having is weight loss and tiredness.
Had one appointment with a new nutritionist, however, most days It feels like the diet she prescribed to me is not enough on calories to support all my daily needs (I’m very active).
I would love to add a morning smoothie at least, but my nutritionist says that she prefers me not to “drink my calories” and instead have more solid small foods to aid my nutritional needs.
Its been quite a journey between different diets and adjusting to managing flare ups and taking it as part of the process. Sometimes It can be isolating, because I can’t eat everything like I used to. I prefer to stay home and cook my own meals for safety.
Currently, I am not taking any meds other than PPI and tums.
I wish I had more pharmacological alternatives, but I took Motegrity for a while, and I experienced many difficulties with side effects, refused to take Reglan due to the possibility of extrapiramidal effects. And since I have not been vomiting for the longest time, I just choose not to take any other medication. However, I’m going to look up on the tummy drops and magnesium.
I don’t take a multivitamin every day because It gave me excessive amounts of vitamins in my body, daily take vitamin c, vitamin d, folic acid.
To every person that has this condition, I am rooting for you, I know sometimes it can be difficult and debilitating, but Life is beautiful and we just have to keep strong and willing to make a lifestyle that works for us and not let our condition define what we can achieve in life!
Hi Natasha,
I am so glad that this brought you some hope! I agree, It can be very isolating to not being able to eat with other people. Sorry I didn’t reply immediately, I’m struggling through some new health challenges but I’ve been thinking about your post.
Does your nutritionist take care of very many gastroparesis patients? I saw a wonderful nutritionist who had a lot of gastroparesis patients and she didn’t have any problem with me doing two of meals as liquids. I’ve heard the “don’t drink your calories” a lot related to weight loss. But with gastroparesis, I think it’s a very common way to get the calories we need because it doesn’t get stuck in our stomach for extended periods of time. I have a friend who did Botox for her gastroparesis and she said “it’s amazing to get energy so quickly from the food I eat.” It makes me wonder if some liquid calories would help with your fatigue and weight loss.
I wish you all the best in figuring out what works best for your body!
This is so interesting! I was diagnosed with GP today. I do not experience the regurgitation. I have actually gained weight but I believe that’s because I am in nursing school and my doctor said stress can irritate a flare up. I was wondering why you choose the whey protein for your shakes?
I tolerate dairy and like the texture and taste. I used to use a plant based one but after using the whey, I just don’t like the texture.
My GP also started during nursing school. I wish you the best… nursing school is hard! As far as the shakes: Soy makes my GP flare and I don’t like the taste/texture of any of the plant-based protein shakes. Since I tolerate whey, I use that because I like it.
May I know what drinks helping u I am lacking calories very sick
Hi Krista!
Thank you for all the info you provided! I was just recently diagnosed with Gastroparesis. This sucks. I’m going to try to cut out coffee too and try more shakes throughout the day vs. meals. Feeling nauseous after every meal is infuriating. Also, have you heard of Gaviscon? That stuff is amazing! Unfortunately, it is originally from the UK but you can buy it at amazon its just more expensive than getting the U.S. version. The U.S. version is not quite the same thing with less efficacy. But I LOVE it, the UK version. Instead of using PPI’s I have been using that. It was recommended by my doctors here in CA.
I’m sorry you have gastroparesis. It does suck! Thanks for the recommendation. I wish you the best as you figure out what works for your body
I am so happy I found your website. I was diagnosed 3 years ago with gastroparesis. Every day is new. What I ate yesterday, or last week, I can’t eat today. Always a struggle. I’ve been looking for a fruit/veggie smoothie mix-in and I am looking forward to trying the brand you recommended. I am going for another stomach emptying test soon as I’ve been getting worse. I am now doing the shakes & one meal like you to see if the nausea will diminish. I hope you post new information as you learn more about what works and what doesn’t. Thank you all for sharing.
Hi TrishA. I’m sorry you’ve been getting worse. In the last year or so I’ve been trying to dig into why my gastroparesis improves with Benadryl but haven’t found any clear answers. Wishing you the best
Hi Krista, I just want to thank you for posting this. A few weeks ago I had a gastric emptying done and my results where 52% ugh. Its been devastating for me at age 51, but after 6 months of nausea at least I know what’s going on. Of course my GI’s nurse not my GI called and said I needed to google my issues and try to come up with diet on my own. That wasn’t very helpful.Your post has helped me so much. I really dont want to eat cooked leafy greens for the rest of my life and im trying to decided on plant protein or whey since dr google says not raw fruits and veggies. Do you eat any fruit ? cooked or raw ? Ive tried celery juice but it upset my stomach….. I may try do a smaller portion of celery juice and see how it goes. have you started juicing yet? Take care
What I eat depends on how I feel on any individual day. Sometimes I can eat more raw fruits and veggies and sometimes it’s a no-go. Right now the raw fruits I eat are melon, strawberries, blueberries. Plus I do fruit smoothies. I’ve juiced in the past since it’s a good way to get the nutrients without the fiber but haven’t had enough energy to do it recently. Wishing you the best as you figure out what works for your your body
Hi my name is Maria
FOR almost 20 years off and on I have had this problem
My primary ordered the gastric emptying test and today it does show slowness we need to confirm with my gastro doctor how to move forward..
I am literally beside myself in tears, I have know idea where to begin,,are there exercises that I can do to help the process?
I noticed that I had taken naproxen last night for back pain and it is bothering me today,,
I also enjoy an occasional glass of wine but i am scared..
PLEASE help,,
Thank u
I’m sorry you’re struggling with this. I haven’t heard of any exercises to help, but remaining upright for several hours after eating allows gravity to help. Wishing you the best!
Hi Krista! My name is Kady and I have been having almost the exact same experience for the last 2-3 months. I’ve always dealt with digestive problems since I was about 12 but it has never been this bad before. How long did you have these symptoms before a doctor diagnosed you? And did you ever get tested for food allergies or intolerances? I have gone to the doctor multiple times for this problem and every time they give me another pill that doesn’t work and tell me to try it for a couple weeks and if it doesn’t work they’ll give me something else.
It didn’t take that long to get a diagnosis. When my EGD was normal, the GI MD diagnosed me with gastroparesis because I was having food come back up into my mouth to when I laid down and was burping up breakfast at bedtime.
A few years later what I was doing to manage it wasn’t working so I saw a different dr who did another EGD and then the Gastric emptying study. I’d suggest advocating for a gastric emptying study if you suspect that is what is going on. It’s the gold standard for diagnosis. I already had known food intolerances prior to developing gastroparesis – nothing that showed on blood work or skin testing though. When I was struggling with that a friend recommended a dietician that did this system: https://www.nowleap.com/leap/
It was hard but SO helpful!
Wishing you the best!
I have idiopathic GP, I was diagnosed in 99, mine got super advanced as we in the US mostly get this from diabetes. I live in Utah, in 2009 they approved subtotal gastronomy for GP. It took me a year to decide this was for me. They do not do the gastric stimulator here, It tends to perliforlate the stomach. It definitely needed to be done as they said my whole stomach was necrotic. I was the first one here for thisI felt better than I had, it’s taken me a long time to fugue it all out but now I help people here that are having this surgery, navigating the waters. I’ve had to do this because my son was diagnosed with GP in 2017 & my daughter in 2019. They were diagnosed as genetic. I’m grateful I went thru it first so they didn’t have to fail all the treatments you mentioned above They went right to treatment.
I’m so glad you found something that was effective for your GP!
I have had GP for about 21 years but the past 10.5 have been the worst. I had to get an Enterra gastric neurostimulator, which helps with nausea but of course doesn’t correct the problem or help the other symptoms. It has been a lifesaver for me though – I went from miserable days full of antiemetics and barely being able to function to being able to treat most of my nausea with alternative treatments. I LOVE Tummy Drops too! I take ginger capsules when my nausea is really bad. I tried it 3 times a day before meals and it allowed me to eat pretty normally but it also caused a lot of bloating and reflux, so now I only take it prn. Deep breathing exercises and psi bands can be helpful too.
I just found your article tonight and I am glad I stumbled upon it. Thank you for the information you have shared! I also use Orgain protein powder, drinks, and bars, so I am excited to try your recipes!
Thanks for sharing your experiences. I’m sorry you have this disease.
My husband struggles with GP as well. He finds it to be hardest that he just can’t eat the foods that others eat. We try to ensure that all foods are prepped the way they need to be but he sometimes will still just eat the other anyway and endure the pain. Any suggestions on how to push through that need? He knows he can’t be eating that way but finds the mental struggle of just “not being able to” a lot!
That’s a great question. And I’m not sure there is an easy answer because everyone’s personality and priorities are different. I’ve tried a few approaches:
* I started imagining a “poison” sign when I wanted foods I shouldn’t have.
* I decided that I wanted to feel better and was willing to do whatever it took to make that happen.
* working on accepting my body as it is. Acknowledging the things it can do, and not just focusing on the limitations it puts on my life.
So instead of feeling like “I’m not allowed” or “I’m not supposed to,” I am making an intentional choice to do what’s best for my body. And then when I make the wrong choice I give myself grace because I’m human.
I hope that’s helpful
Great share! I recently found out during a 2nd colonoscopy I have a redundant colon…longer than normal and loopy. Reading about it I learned digestion takes longer. I haven’t been GP diagnosed but I can’t help but wonder if it might be related for me. I have many similar symptoms. Thank you!
Krista, I can’t thank you enough for such an informative, helpful post! Reading about your experience certainly mirrored mine and I’m sorry you had to go through such an experience to finally find what works for you and sharing your story to hopefully benefit others. Granted, I still have a ways to go but relief that there are finally answers and I’m not going crazy! After battling severe, debilitating symptoms for the past 2 years, I finally received the diagnosis of severe gastroparesis today. My number is 60% of food remaining in my stomach after eating which feels such. It has been quite the journey involving a “team” of dedicated medical professionals who worked hard to solve the mystery as you are right in that symptoms for various GI issues are so similar. I know that each person is different and I too will have to figure out what foods I can and cannot eat and work for me. But just reading your account, I don’t feel so alone in this battle. It’s quite the wake up call for this “foodie”. I never thought I would see the day where I would finally get confirmation that my symptoms are real. Unfortunately I fall into the category of unknown cause but at least I now have a name and can now begin the journey of managing it. Thank you again and wishing you continued good health and recovery and management!
Sincerely,
Catherine Oliva
I wish you the best as you figure out managing this disease. After multiple years I realized that mine improved with Benadryl. No provider understood why this was the case. I ended up with other medical issues and was diagnosed with MCAS. When I started ketotifen (a mast cell stabilizer) my gastroparesis improved.
Please give details about taking Benadryl. When, amount, how often
I’m sorry you’re dealing with this disease. Personally I’ve found talking 50 mg of Benadryl at bedtime for a few nights to be helpful when I have a flare. I’m not giving medical advice just sharing my personal experience. Wishing you the best
I was diagnosed I think 6 years ago and also Barret’s esophagus and I also had IBS before being diagnosed and GERD. In the last year though I can feel my body getting worse than what it was. My gastro Dr has never pointed me in a direction of what’s good justfor me to say what I think is ok or not. I’ve seen 2 dietitians that just told me to eat what I want but use a toddler plate. It’s hard for me to figure things out when I work as a manager in a customer service type job and my shifts go from day to night and I only get one break during that time so meals are very hard for me to figure out as well even snacks because always on the move and helping customers. I am tired constantly, am bloated and my abdomen is always distended and I’m in pain alot of the time. I get nauseous randomly and constantly go from constipation to painful muscle spasms with diarrhea. I do know that mornings are my worst and by the evening I can finally eat ok but I feel starved and want to eat everything which I believe is what makes my mornings bad but with my work schedule I don’t know how to change it. Any suggestions from anyone would be most helpful. I would love to feel something other than this misery.
Thank you for this information. I was just diagnosed with gastroparesis, but have been existing f with it for several years. I look forward to trying some of your suggestions to get some relief. I had a really bad night last night. It was my fault for eating too much too late in the day. I’m miserable today. My throat is raw from the nausea I experienced last night followed by severe acid reflux thar lead to vomiting last night. I wan these episodes to stop so I’m going to try everything I can to be successful. The foods the doctor recommended aren’t really all that great for my diabetes which I was diagnosed with earlier this year so I feel like food is my enemy. I can’t eat any kind of dairyman, almond, or soy products without experiencing distress so it’s a challenge to find things I can eat. I’m ordering the cook book you recommends and am looking into some of the other products you’ve recommended. Thank you for sharing your knowledge.
Trish, I’m sorry you’re suffering with this disease. Wishing you the best as you figure out how to manage your body!
Hello I took this when I had my gallbladder out 3 years ago been in lot pain withbit my liver in large an cyst on my pancreas don’t know if this can do all this are not in lot of pain with flair up I use ginger snaps a lot please get back with me thanks
Hi Francis, sorry for the delay in responding. I’m so sorry you’re in so much pain. Hoping you find a solution that helps.
Krista, I wish thank you was enough to say for this post! I’ve learned more from your article than I’ve learned since my dx over 8 years ago. Thank you! I have GP, GERD, IBS, Barrett’s Esophagus and a rare form of Muscular Dystrophy. I have had numerous EGD’s and Colonoscopies. I suffer from occasional constipation and have diarrhea more often than not. I take a PPI, Protonix. I use Mylanta and Tums as needed. I see a Gastroenterologist. We are talking about seeing a nutritionist for a diet plan. I also have type 2 diabetes caused from pregnancy it went undetected. I can’t do Reglan because of some of the side effects, i.e. Tardive Dyskinesia. My muscles are already compromised from the MD. The doctor is trying to figure out what would help with the GP that won’t affect the MD. I’m trying my best to manage with diet. We have talked about a stimulator and/or feeding tube eventually. It’s definitely a hard thing to figure out. My heart breaks for anyone having to deal with this. Blessings! Thanks again for all of the information!!
I am so sorry you have this disease! I’m glad this information was helpful. A friend had Botox to the pyloric sphincter and it helped significantly. I also have POTS which requires a ton of oral fluids and I’m struggling to drink it. I’m going to be asking for a JG tube. Not sure if my gastroenterologist will say yes, but I figure it can’t hurt to ask
I can’t do intermuscular injections of any type because of the MD. I’m hoping at my July appointment my gastro will have some type of answers for me. Fingers crossed!
Just diagnosed- thx so much for the info, especially tummy drops. I am diabetic so found a sugar free brand online. I eat one small meal and one or two snacks per day ( all soft and vegetarian). I can’t eat until at least noon or later. Hoping I can manage without taking the meds. Time will tell.
Wishing you the best! It looks like I’ll be trialing domperidone soon.
Thank you so much, Krista. After doing very well with MS due to significant mindfulness to food for more than 20 years, gastroparesis has developed. It’s fairly common to MS. But, like others here, my dietary reality has completely changed in one fell swoop. So, your post has really helped put the lists from medical sources in perspective. And, your personal go-to’s are a blessing. Thank you again. I hope you are doing well.
I’m so glad it was helpful. Send you my best wishes