Last week, I spent some time last week reading through PPE recommendations from the CDC, WHO, WSHA, Washington L&I, WA DOH, and UW. At that time, CDC and WA L&I both recommended airborne precautions when caring for all COVID patients regardless of what type of procedure was being performed. WHO, WSHA and UW only recommended airborne precautions when doing aerosolizing procedures. DOH recommended airborne precautions for aerosolizing procedures and “critically ill” patients.
Today, a friend asked the question, “Do you think essential workers are getting the best PPE that can be provided?”
The answer is “no.”
Normally in healthcare, we default to the safest option until other options are proven.
“Best” PPE would be us saying “there are indications that this could be airborne, let’s protect our workers/ourselves until it’s definitively proven otherwise.”
“Best” PPE would mean disposing of disposable PPE after using it with one patient one time.
It would mean laundering reusable gowns after one use and never having to reuse a gown another healthcare worker already wore in a COVID patient’s room.
It wouldn’t involve cloth masks – which have varying levels of filtration depending on the material used but most are not as safe as surgical masks.
It would not require workers to reuse the same PPE for an entire day or an entire week or an entire assignment.
“Best” PPE would not involve differentiating between aerosolizing procedures and the rest of a patient’s care.
“Best” PPE would not cause healthcare workers across the country to feel afraid to go to work because they don’t have the tools they need to protect themselves.
“Best” PPE would involve engineering controls that also keep us safe, like using negative airflow whenever the patient is suspected of COVID, not just for aerosolizing procedures.
Let’s say “good enough” PPE is the next step down from “best.”
“Good enough” PPE would involve extended N95 use (wearing one time without taking off for an extended period of time) AND discarding N95 after use in an aerosolizing procedure (per CDC recommendation). It would not involve using the same N95 for multiple aerosolizing procedures.
“Good enough” PPE would involve N95 reuse within limited circumstances AND wouldn’t involve placing it into a container (like a paper bag) that can easily contaminate the side that faces the health care worker.
Below “good enough” would be “inadequate.”
“Inadequate” PPE is using trash bags as gowns.
Or only having access to a surgical mask that is reused for days on end, that the healthcare worker reinforces with feminine hygiene pads to prevent it from disintegrating
Or only having access to cloth masks or reusing cloth masks over N95s.
We are in a shortage, some of it happening in real-time and some of it based on projections. But we can do better.
We may not have the “best” PPE right now, but we can do better than “inadequate.”
And the organizations that outline recommendations can do better at communicating the WHY behind their changes or differences. Please, share the evidence and explain your reasoning with us. We’re trained to evaluate recommendations based on evidence, please show us the evidence.
In the future, we need to plan better.
As a nation, we need to champion for our government and our local healthcare facilities to have a reserve of equipment… because we are showing our enemies how susceptible we are to bioterrorism.
But we can do better now.
Krista, RN, CEN, TCRN
P.S. I think this idea for using rubber bands to help “seal” surgical masks to our face is pretty cool: Fix the Mask
P.P.S. I work at multiple facilities and have friends at many other facilities. These opinions are generalizations of my observations and are not about any specific facility.
P.P.P.S. It’s strange that employers are defaulting to recommendations that aren’t aligned with L&I recommendations since L&I are the people who decide whether an occupational claim is appropriate or not. I would think from a “protect the organization from liability” perspective that the L&I recommendations would be the go-to source.
—————
Relevant quotes and summaries from sources as of 4/1/2020
WA L&I “ When available, an N95 respirator is preferred to ensure workers are protected from any contamination residual in the air… N95s are the minimum level of respirator filtration but provide effective protection from known COVID-19 exposure.” They also recommend that if reuse of N95 becomes necessary it should be done cautiously and according to CDC recommendations
CDC differentiates between extended use and reuse, “Extended use is favored over reuse because it is expected to involve less touching of the respirator and therefore less risk of contact transmission.”
- https://www.cdc.gov/niosh/topics/hcwcontrols/recommendedguidanceextuse.html
- https://www.cdc.gov/coronavirus/2019-ncov/hcp/healthcare-supply-ppe.html
- https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html
Note: many of these URLS now redirect to different pages
Washington Department of Health “We acknowledge that the CDC currently recommends standard/airborne/contact precautions with eye protection for patients at highest risk and we continue to support this approach for our patients who are critically ill and those undergoing aerosol-generating procedures. These CDC guidelines also recognize that based on local and regional situational analysis of PPE supplies, facemasks are an acceptable alternative when the supply chain of respirators cannot meet the demand.”
World Health Organizations lists droplet/contact precautions and only N95 for aerosolizing procedures
Washington State Hospital Association is copying WHO and states they aren’t following CDC guidelines
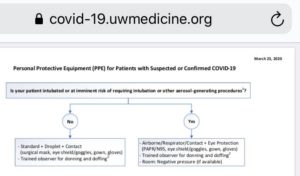
The University of Washington Medicine is also limiting airborne precautions to aerosolizing procedures. Although they also do something I haven’t encountered in my reading: “PPE use for suspected or positive COVID cases will continue to require a trained PPE observer to assist with donning and doffing.”