-
COVID-19: Are essential workers getting the best PPE?

We may not have the “best” PPE right now, but we can do better than “inadequate.”
-
Life after nursing school
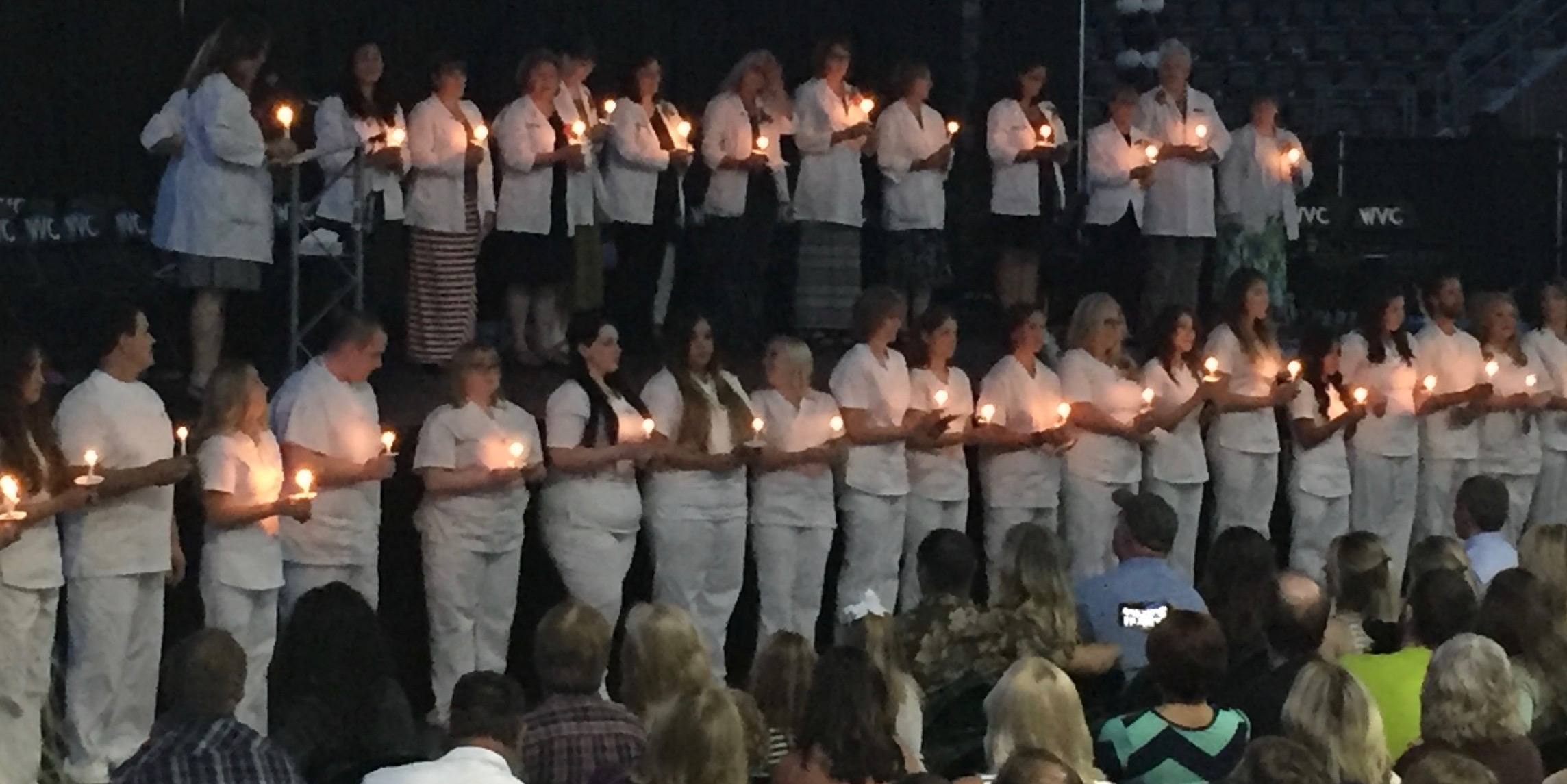
The countdown to the end of nursing school is underway. My last exam is June 14th and pinning is June 16th. I can’t believe we’re here! It’s hard to believe that 3 years ago I was plotting away with absolutely no idea that I was going to embark on a new career path in healthcare. […]
-
Nursing Pharmacology: Adrenergics & Cholinergics
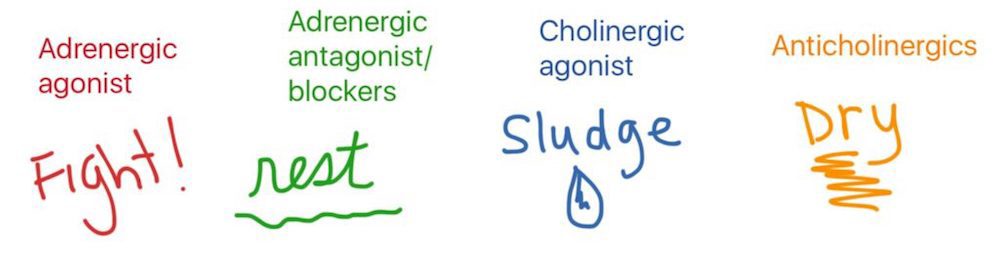
I had a love/hate relationship with nursing pharmacology for my first year of nursing school. I loved the information but hated learning it. I didn’t figure out how to learn it effectively until we were 70% finished. Since then I keep thinking, “there has to be a better way to learn nursing pharmacology.” I recently […]
-
Why I chose nursing
A few years ago I was working late when a co-worker said, “Why are you still here? It’s not like we’re curing cancer.” The reason was simple: it’s in my nature to focus intensely and invest significantly regardless of what I’m doing. This conversation prompted questions like: Am I making a difference in the world? […]
-
If I was my patient, how would I feel?
THEY say “Remember apple, table, coin.” Apple. Table. Coin. I am angry. You would be too. Try not being able to speak. Attempt to communicate and cause only confusion. Try wearing a brief. Sit in your urine and wait. Then in your feces. And to make the indignity worse Allow a stranger to invade your […]
-
Humans not diagnoses; Reflecting on CNA clinicals
This summer I took a CNA class in preparation for nursing school. Here’s what I learned. Our patients are not just diagnosis. They are people. They have a history. Their feelings and experience—both past and present—matter deeply. I can imagine that it becomes easier to see them as tasks to perform instead of people to […]
-
Next stop: nursing school!
Thought I’d post an update on where I’m at with “going back to school and completely changing careers”. I start Nursing School at Wenatchee Valley College in 17 days! It’s a 2-year ADN (Associates of Nursing) degree. As preparation, I completed a CNA course over the summer. I walked into class saying “I’m not sure […]
-
How fats we eat become energy in the body
The farther I get into organic and biochemistry the harder it is to find information that uses minimal jargon, helps me find the big picture amidst thousands of details, and that connects the biochemical concepts with what I’m learning in Anatomy & Physiology. So, I decided to post what I recently learned about how the […]
-
Medical insurance, pre-existing conditions and Obama care
When I went back to school to finish my Bachelor’s degree several years ago, my COBRA payment was somewhere around $450 per month. Due to a pre-existing condition I didn’t qualify for any less expensive options. After graduation I worked as a freelancer. Taxes alone required saving approximately 50% of my income, which meant I […]