-
Living with gastroparesis: my experience with diet, foods and medications
I have gastroparesis. Gastroparesis is a condition that affects the normal spontaneous movement of the muscles (motility) in your stomach. Ordinarily, strong muscular contractions propel food through your digestive tract. But if you have gastroparesis, your stomach’s motility is slowed down or doesn’t work at all, preventing your stomach from emptying properly. –Mayo Clinic For […]
-
Why I chose nursing
A few years ago I was working late when a co-worker said, “Why are you still here? It’s not like we’re curing cancer.” The reason was simple: it’s in my nature to focus intensely and invest significantly regardless of what I’m doing. This conversation prompted questions like: Am I making a difference in the world? […]
-
Next stop: nursing school!
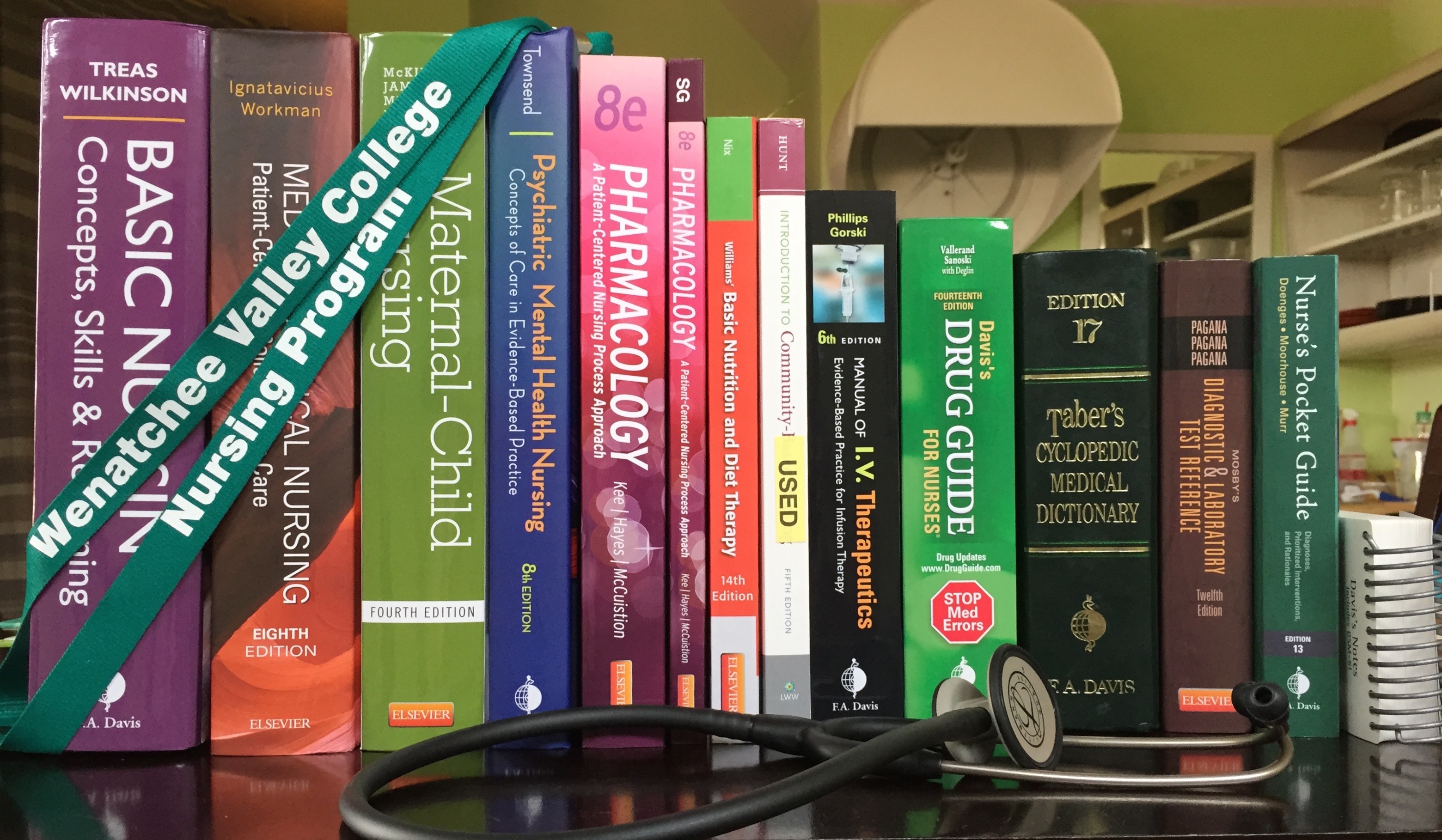
Thought I’d post an update on where I’m at with “going back to school and completely changing careers”. I start Nursing School at Wenatchee Valley College in 17 days! It’s a 2-year ADN (Associates of Nursing) degree. As preparation, I completed a CNA course over the summer. I walked into class saying “I’m not sure […]
-
What’s next on my midwifery journey
Hi friends and family! As I shared in September, I am on a journey to become a midwife. I’ve wrestled through the decision on what training and credentialing to pursue and even took a little sidetrack exploring medical school. But I’ve settled on the decision to become a nurse-midwife. This means I’ll become an RN […]
-
Responding to grief
I wrote this letter recently for a dear friend who is heading to the Philippines to train as a midwife and who asked for “read me when” letters. I had no intention of sharing it with anyone else at the time. But there are two reasons I’ve decided to do so: Last night I learned […]
-
Medical insurance, pre-existing conditions and Obama care
When I went back to school to finish my Bachelor’s degree several years ago, my COBRA payment was somewhere around $450 per month. Due to a pre-existing condition I didn’t qualify for any less expensive options. After graduation I worked as a freelancer. Taxes alone required saving approximately 50% of my income, which meant I […]
-
Blank contracts and the faithfulness of God
Wesley Covenant Prayer: I am no longer my own, but thine. Put me to what thou wilt, rank me with whom thou wilt. Put me to doing, put me to suffering. Let me be employed for thee or laid aside for thee, exalted for thee or brought low for thee. Let me be full, […]
-
A voice cries out
I wrote this initial part of a blog in October 2012: I’ve thought about blogging for years. In 2008, I was asked to write a guest blog for Renee Fisher, and I loved it. I wanted to do more of it. But something always got in the way. That something was the belief that what […]
-
Giving out of poverty
What is it like to give everything you have left? Have I ever truly done that? I’ve been asking myself this question for a few days. And not really about money but about my time and energy because that is the “currency” that I really value and when it’s running low I conserve instead of […]
-
Confessions from failure
To wrap up my reflection on my short time in the Army, here’s a short piece I wrote a few years ago: Reminders There are many things that remind me Of the failure in my past. The smell of gunpowder in the air which follows the crack, crack, burst of the rifle. The burning in […]